The last few weeks have been stressful with no news and, as a result, no plan. Finally, at 36 weeks, we now have one, but it might not be the plan everyone was expecting us to have. If you haven’t read our previous post about our pregnancy journey so far, you can read the last one here.
From the start, we always knew that I’d require some sort of medical input when it came to labour time and birth. Our biggest fears were that I’d be pressured into accepting a c-section which for me would mean a difficult recovery and relying on Alex and our families for almost everything for the first 8-12 weeks, both in terms of my care and little one’s. I’ve always been for a physiological birth, or as close to it as I can possibly get, only going for a c-section or other interventions if absolutely necessary, especially as it would very likely need to be done under general. Luckily, the result of the MDT meeting was that if I don’t want an elective c-section, then I don’t have to have one, but it’s under the condition that I’m aware we could still be heading down that route if either little one or I don’t cope well in during labour.
How the option of induction came about and why we accepted
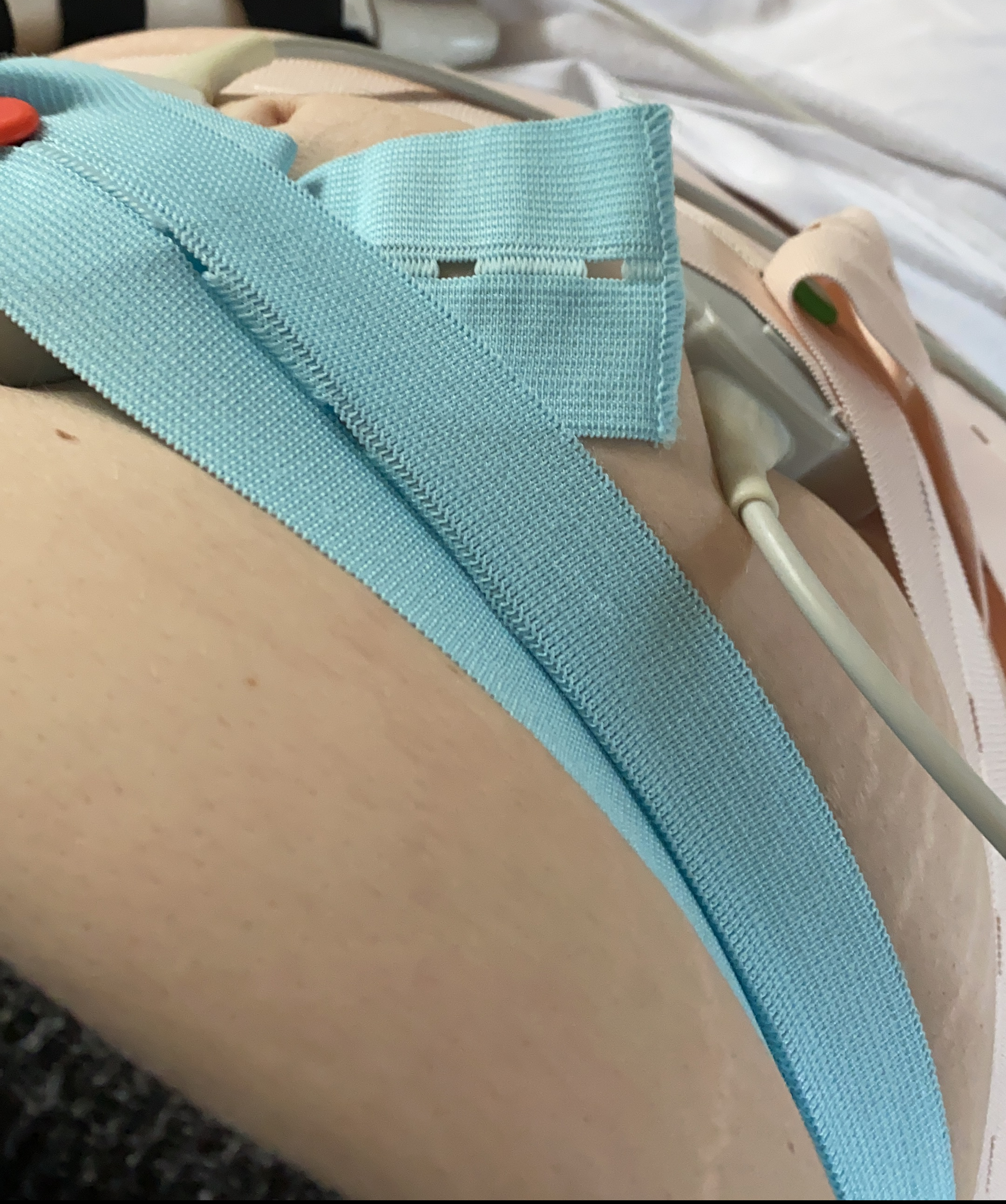
One of the biggest things about not going down the c-section route is unpredictability and the risks involved. For us, not only do I have a medical condition which means I can’t feel movements or contractions and have to palpate for them, but I’m also at risk of precipitous labour. Then, to top it off, we found out that I have Group B Strep at 26 weeks, and I’m also at risk of other complications. It meant that the idea of induction was proposed to us, with all the risks and benefits involved. Benefits? We’d have an idea of when my labour will begin, and with it, the option to ensure Alex is off work for a few days so that he doesn’t miss the birth. It also eliminates the risk of me giving birth at home with no help other than Alex’s Avmed training, which, whilst the scope of what Avmed covers is fantastic, where childbirth is concerned, it doesn’t equip you for a complicated labour birth. Cons? If it fails or something else happens, it’s a c-section since assisted delivery via forceps or ventose is out of the question due to dislocation risk. It also further increases my haemorrhage risk, something my consultant already factored in early on so that there’ll be medication drawn up and on standby if it’s needed.
As my midwife talked to me about induction some weeks ago when Alex’s roster and being back at work was causing me stress around whether or not he’d even make the birth, Alex and I had actually spoken about the possibility of induction. We researched the risks and benefits before my consultant had even offered it to us to come to a decision together without feeling pressured. After those discussions with Alex and my midwife, I said that if induction was offered to me, I’d accept it to reduce the risk of that happening as him not being at the birth would be heartbreaking for us both. It also gives us some control over the situation as long as little one stays put and I don’t go into labour before induction day, something which could happen and my consultant warned us about when we accepted the offer. Alex had already made it clear that he’s scared of waking up during the night to find me still asleep whilst in advanced labour, something which we both know would affect him massively even with all of the training he’s equipped with, thanks to him being crew!
As you can see, accepting an induction of labour was an easy decision for us once we’d weighed up all of the risks and benefits. Even with the risk of having to go down the c-section route if something goes wrong, the thought of having an unattended labour and birth with all of the dangers attached due to my complex medical history scares Alex and I more. We are also fortunate that we never felt pressured by the team looking after us to accept induction, mainly because we’d had that discussion ourselves beforehand, giving us time to fully consider everything. Not only is there information on induction of labour available to read in my handheld notes, but we also turned to Google to research the specific risks that are unique to our situation and spoke to other pregnant people who have EDS. But what if you’re enjoying a lower risk pregnancy and offered induction, or just don’t know if you want one?
Research is your best friend.
Alex and I both know people who have been offered induction of labour and felt little pressure to accept, as well as plenty of people with low-risk pregnancies who felt forced into accepting an induction to keep their team happy. We started looking into our options quite early on once our consultant told me that she’d do everything possible to keep our options for labour and mode of delivery open. That kind of support from her when every other specialist outside of obstetrics had told me that c-section was the safest way forward meant the world to both of us. It also meant that we felt even more supported by the teams looking after us, both at our local hospital and the Silver Start Unit in Oxford, who we’re so thankful to have the specialist input of.
Great places to research induction include Google (especially as you can tailor your search to your unique situation) and your handheld notes if your hospital provides information on induction of labour in these. I also highly recommend speaking to people who’ve had an induction of labour offered about their experiences, even if they didn’t accept the offer, as firsthand experiences can often help the decision making process. This same piece of advice goes for those who have medical conditions which could influence management. There are plenty of online groups on Facebook etc., which allow you to connect with others going through similar! If you can, start researching and discussing your thoughts with someone else early! This means by the time an offer of induction is given to you (if it is), you’ll have already thought about it and either decided on whether or not to accept, or you’ll have an idea of what questions to ask. It also means that whatever your decision is, you’ll be able to explain the reasoning behind your decision to whoever is looking after you knowing that you’ve given yourself time to consider all the risks and benefits. I’ve also learned to use one acronym that has helped us massively with each decision we make, called B.R.A.I.N.
What is B.R.A.I.N?
B.R.A.I.N really is what it says it is; it’s using your brain to make an informed decision.
B – Benefits (what are the benefits of this test or procedure for me and my baby?)
R – Risks (what are the risks of this test or procedure for me and my baby?)
A – Alternatives (What, if any, are the alternatives?)
I – Instinct (What is my instinct telling me? What do I think and feel about this test or procedure? Who else can I ask about it?)
N – Nothing (What could happen if I decide to do nothing or wait and see? Can this test or procedure be delayed? Can I take some time to think about it or research?)
B.R.A.I.N is something we’ve used throughout our pregnancy journey to make informed decisions and choices that we know are right for us without feeling pressured into doing something we may not necessarily want to do. It’s also something that we will continue to use and advocate that others use, especially as it is such a handy tool to have. With the NICE draft guidelines meaning that an increasing amount of people are already being offered induction at 39 weeks even if there isn’t a clear clinical need, now more than ever, birthing people and their partners must be able to make informed decisions without feeling pressured into accepting something they may not actually want.
Have you been offered an induction of labour or had one in the past? Feel free to share your experiences in the comments with us!