TW: This post details our NICU journey and the reason why our baby needed NICU.
Following on from our birth story blog posts, it’s time to introduce our little one to you all, as well as what happened next!
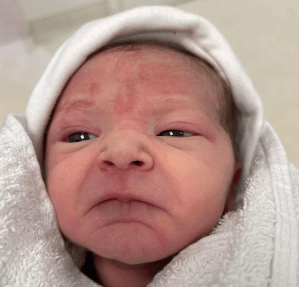
Our little miracle and fighter, Alice Frances Margaret, was born at 0710 on 21st August 2021, weighing 2480g. She came into the world face up, which meant the first of Alice’s many facial expressions we were greeted with was her extremely grumpy one which Alex managed to get a photo of.
Perfect in every way, I was so glad to get some skin to skin with her. However, my right arm had been severely affected by the epidural, which meant I couldn’t lift my arm or move it very well, so Alex and Paige, the midwife who took over from Sarah shortly after Alice was born, had to help me with holding her. All was going perfectly until 79 minutes after Alice’s birth.
People always say expect the unexpected, but what happened at 0829 on that Friday, just 79 minutes after Alice’s birth, shook both Alex and me to our cores. It really was the worst moment of our lives so far, as Alice stopped breathing while on my chest, and we didn’t even realise it. I genuinely thought that Alice had fallen asleep on my chest. Even when I mentioned it to the nurse looking after us in recovery in search of reassurance, the fact that she didn’t respond made us both think it was ok. It wasn’t until Paige came back in 30 seconds later and realised what had really happened that all hell broke loose.
Having your baby swiftly taken off of you and seeing medical staff resuscitate them whilst the emergency buzzer means more medical staff are swarming into help is something that neither of us would wish on our worst enemy. I honestly thought we’d lost our baby, and Alex was that focused on trying to see what was being done to Alice that one of the staff had to try and force him to come and comfort me as I was being pushed out of the bay to a different area of recovery. We had no idea at that moment in time if our baby would make it. The 15 minutes it took to find out the update was the longest 15 minutes of my life. It truly felt like hours.
The doctor who came to give us the initial update on Alice happened to be one of the doctors who looked after my mum in 2013 when she was fighting for her life in ICU. The second he said Alice was breathing, I felt the most enormous wash of relief pour over me. It didn’t matter that they were still trying to stabilise her and that the neonatal team were transferring her to NICU at that point, she was alive, and that was all that mattered.
Shortly after the initial update, I was transferred back to the labour ward, and Alex came with me. At this point, I was trying to process exactly what had just happened to us, but if I’m honest, my brain couldn’t take anything in. As soon as I saw my dad and he realised that Alice wasn’t with us, I burst into tears once more because I couldn’t get out exactly what happened and Alex had to tell him for me. It would be another 24 hours before my dad met his first grandchild, as our NICU had a rule that grandparents could only visit on weekends in the afternoon due to covid. Still, it was a lot more lenient than most NICUs in the UK. At the time of writing this blog post, some weren’t even allowing parents to visit their child/ren together.
Soon we received another update from the doctors working on Alice, and with them came the news that our baby was finally stable but not yet out of the woods. One of us was allowed to go and see her, but I couldn’t push myself in my wheelchair, so I told Alex to go down and get lots of photos and videos for me until I could go myself. As upset as I was that we weren’t going together, I knew that Alex would be able to prepare me for when I finally got to see Alice. After Alex got back, we were moved to postnatal, so I sent dad home to get some rest before bringing the colostrum we’d harvested to the hospital. I was an absolute hot mess, so before going to neonatal myself to check up on Alice, Alex helped me get showered and changed. He then briefed me on all the rules and what to expect, but if I’m honest, nothing could have prepared me for what I was about to be wheeled into.
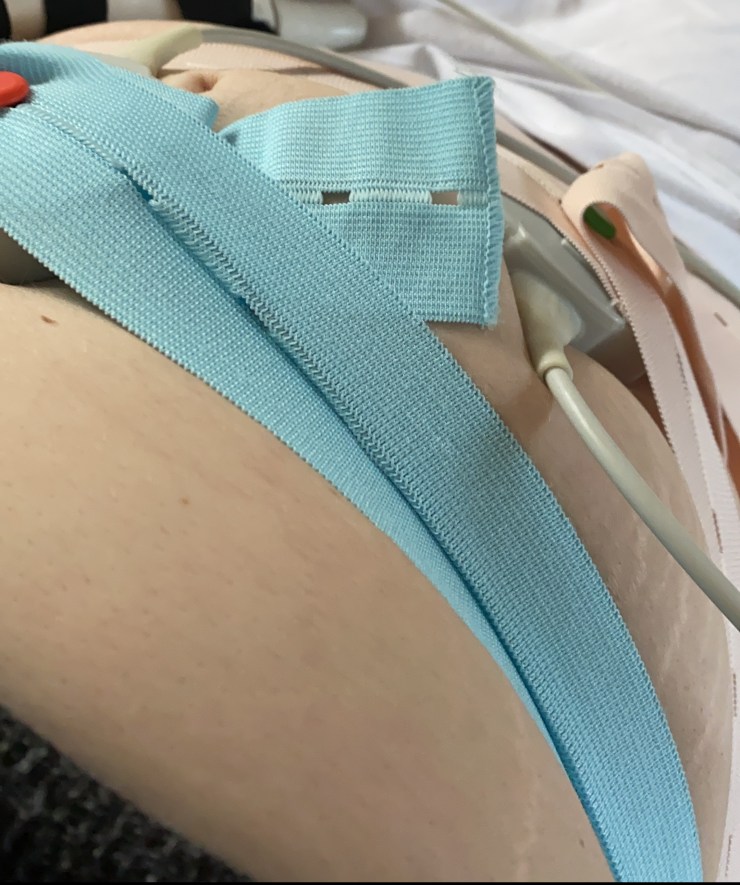
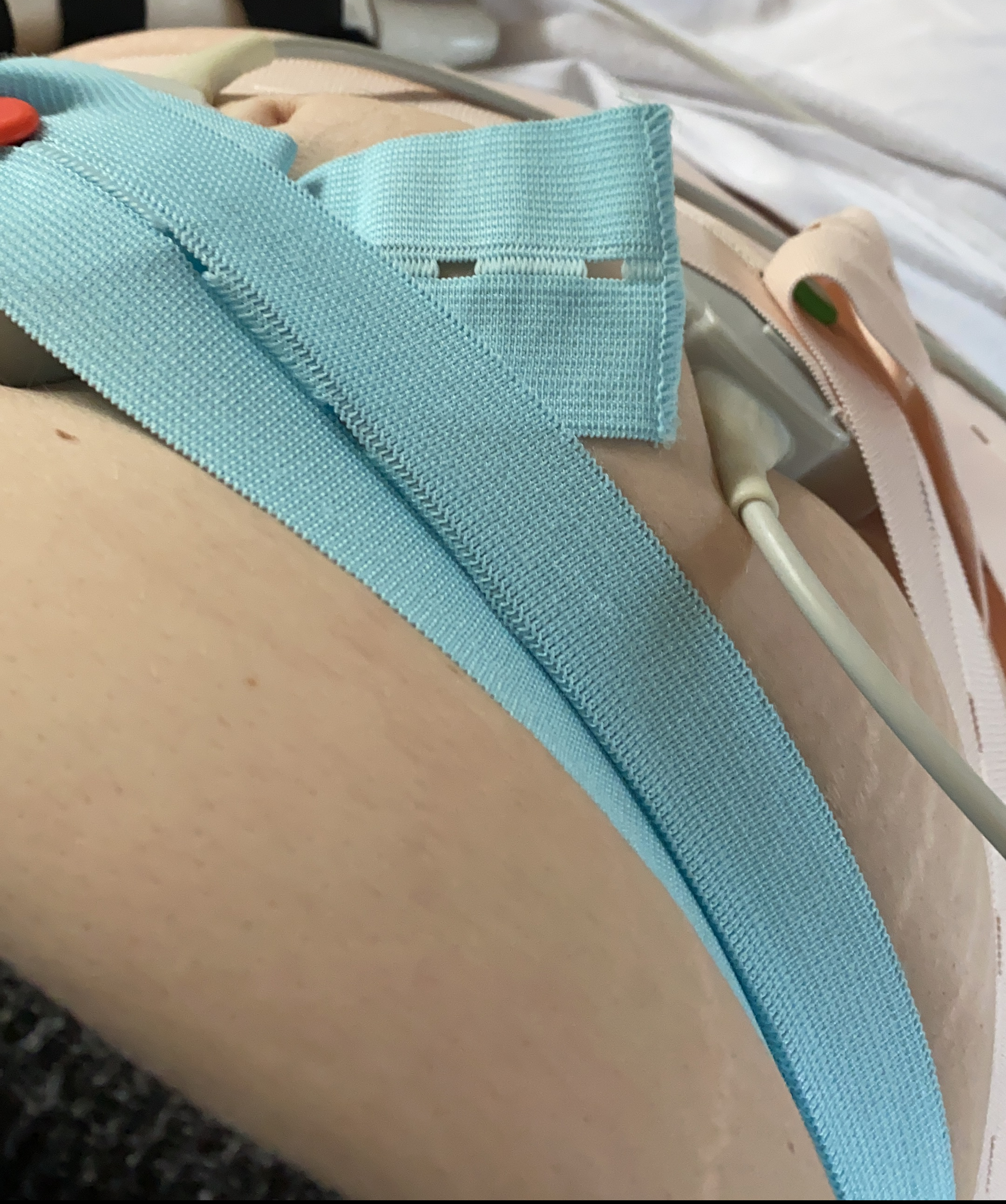
Having a baby in NICU is something I wouldn’t wish on my worst enemy. Seeing your child so unwell and not being able to hold them is tough. Once Alex wheeled me down, and we’d both washed our hands, he took me over to Alice. She looked so unhappy, which make me shed tears once more. She was covered in wires, hooked up on oxygen and on fluids. Her incubator felt like this massive barrier; I couldn’t hold her or do skin-to-skin to comfort her. It was a far cry from how everyone expects the first few hours after giving birth to go. Thankfully, one of the nurses came over to ask if I wanted to put my hand in and comfort her that way, which I jumped at the chance to do. I felt awful for Alex, who couldn’t hold or touch Alice the entire time she was in NICU. It wasn’t until Sunday, when Alice was on transitional care, that he got to hold her for the first time since she’d stopped breathing 2 days earlier. On the other hand, I got my first cuddle on Friday night whilst being able to feed her. However, it was filled with anxiety as the position I had her in for feeding was the same position she was in when she’d stopped breathing 12 hours before.

Although Alice was out of NICU after 40 hours, followed by 2 days on transitional care before going home, those 40 hours taught me so much about a world few know about. Being NICU parents really showed Alex and me just how strong we are, even if we doubted that strength before. Before going home, we managed to catch up with Paige, the midwife who literally saved Alice’s life and between her and the neonatal doctors got as much information as we could. Unfortunately, not all the questions were answered; we’ll never know the reason why Alice stopped breathing. The fact she did in the first place shocked even the team looking after us, especially as Alice had an Apgar score of 9 just 1 minute after birth and then a perfect 10 at 5 minutes. A few have asked us if my Group B Strep infection caused it or if the reduced fetal movements played a part, which again is something we’ll never know. However, although we were fully covered with antibiotics for Group B Strep, Alice’s infection markers were raised when checked, so she was placed on IV antibiotics for a few days as a precaution. Since we’ll never know what caused her to stop breathing, we have been warned it could happen again. It’s something I constantly hope doesn’t happen, but if it does, Alex and I both know how to resuscitate babies and infants thanks to work.
September is NICU Awareness Month, and we’re so proud of our little fighter who made it through. We’re forever thankful to all the staff who worked on Alice and got her well enough to come home as quickly as she did. We’re also grateful for the support of Bliss, a charity here in the UK that provides information and support to parents of babies born premature or sick, as well as research into improving care and treatment.