With induction day looming (and potentially being brought forward after the last few days of yet more reduced movements), I’ve been preparing more for what I want to use during induction and labour to help me through. However, with multiple allergies meaning that most forms of pain relief are out of the question, I’ve ended up looking for alternatives to use which will help me through. Although I’m unable to feel from the top of my naval below, which means I won’t feel contractions and can only palpate them, I can get redirect headaches if there are any painful stimuli below my naval. Worse still, they can spike my blood pressure if it’s not controlled – something you don’t want happening in labour!
So what am I planning to use?

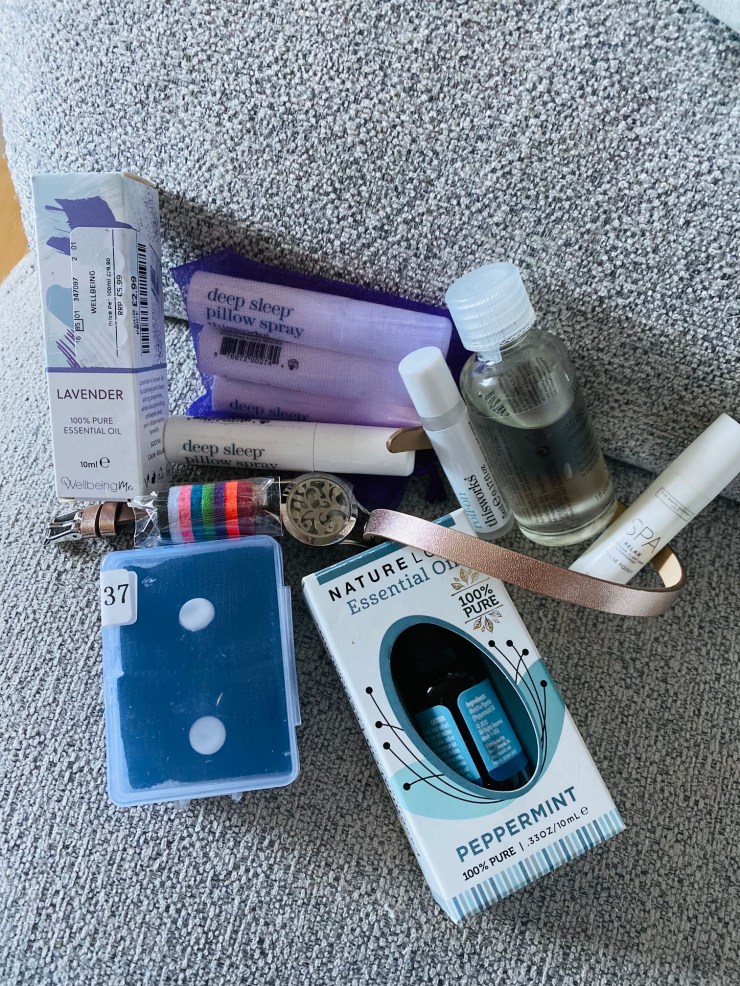
Aromatherapy: I’m a massive fan of aromatherapy. Despite having brittle asthma on top of everything else, I often use aromatherapy to relax and calm myself. There are some essential oils that I cannot use as they set my asthma off big time, but others work really well. Products I adore using include Aveda’s Stress-Fix Composition Oil. This oil is so versatile that you can use it in the bath as a bath oil, on its own as a massage oil, or just warm up a few drops in your hands and breathe in to relax. Unfortunately, it has clary sage in meaning I haven’t been able to use it during pregnancy. However, it is safe to use in labour, meaning that Alex will be on massage duty!
Another duo that I often use, especially when travelling, is the This Works Choose Sleep Bundle. This pillow spray and roll-on combination is a dream! The Deep Sleep Pillow Spray really helps to send you into a nap, whilst the Stress Check Roll-On contains a mix of essential oils to help you fully relax. I also recommend getting an additional pillow spray if you’re being induced, especially as some inductions can take a while, and you’ll want to get your sleep in whilst you can!
I’m also putting in The White Company’s Relax Pulse Point in my case to work alongside the This Works Stress Check Roll-On. Although they do similar things, they have different essential oils. The pulse point contains the perfect mix of lavender, clary sage, and peppermint. This combination is said to be perfect for helping you relax whilst also speeding up labour, plus reducing sickness and headaches.
As well as using aromatherapy blends like those above, I’m also taking pure lavender and peppermint oils to use in an aromatherapy bracelet. This bracelet has felt discs that you pop a few drops of oil on, then place in the disc holder on the bracelet. This is an excellent option if you find that putting oils directly on the skin irritates you, as the oil doesn’t come into direct contact with the skin. You can also use the oils in a diffuser. Some hospitals have diffusers on their labour wards or in the birth centre, so it’s worth asking your midwife about whether or not this is something they provide. Also, some hospitals require you to use their stock of oils, but you can choose which oils you want to use, so you may not be able to use your own oils with the diffuser if they do provide them.
Other non-medical options: As well as my combination of aromatherapy products, I’m also taking sickness bands in with me, just in case. Even though I’m still on a powerful cocktail of anti-sickness medications to control my sickness, there are still some days I use the bands on my ankles as well as my wrists.
I’ll also be using the relaxation techniques and breathing exercises that I learnt through watching The Positive Birth Company’s videos on YouTube. I also have some of their affirmation cards packed ready to go for during induction if I need a pick me up! They also have an affirmations function on Alexa, which I use at home each evening. However, if you download the Alexa app, you’ll be able to use them on your phone at the hospital as well!
What About TENS or water?
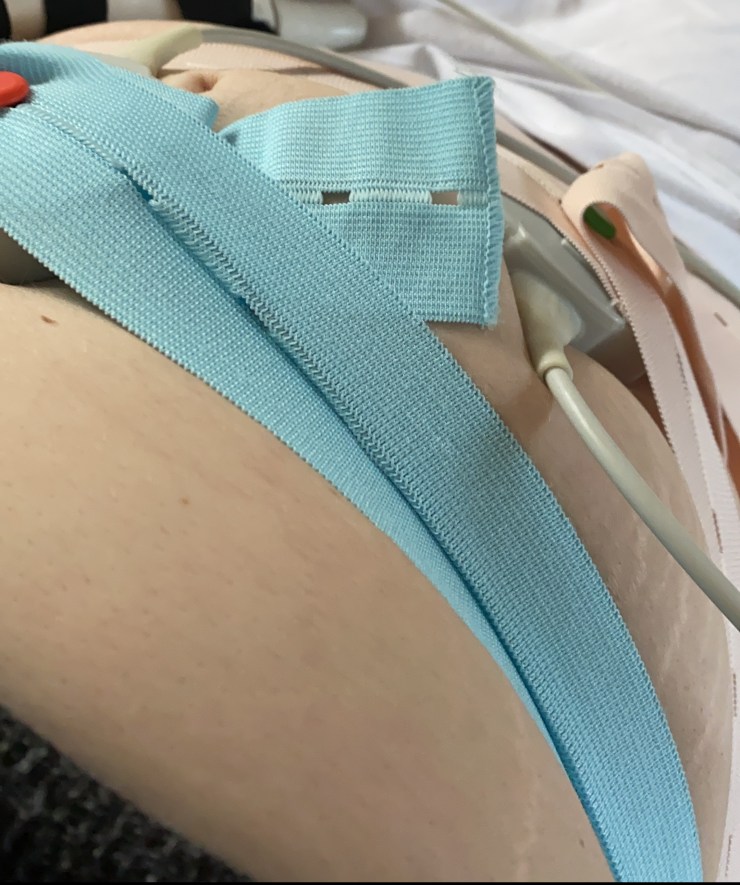
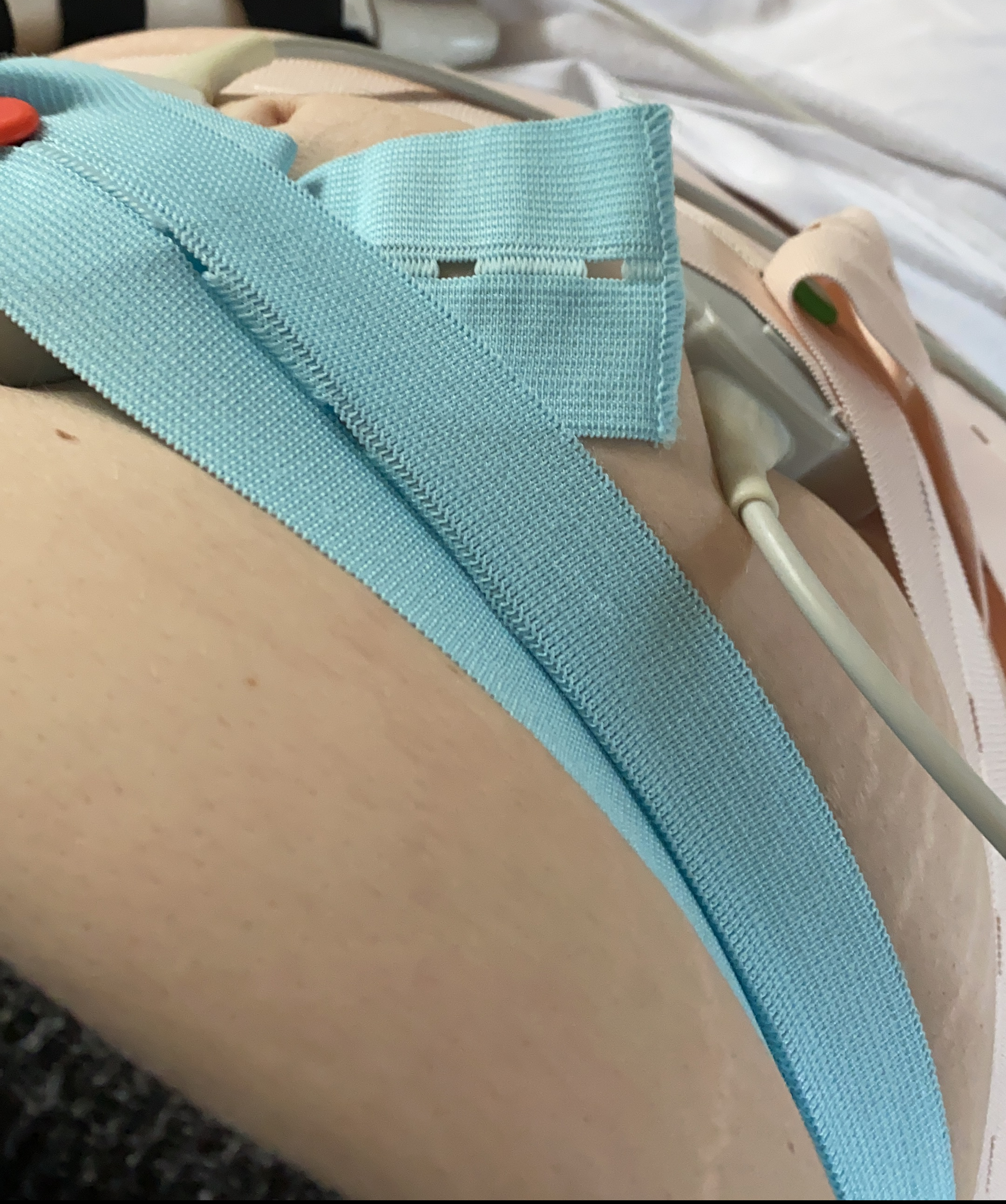
Unfortunately, because of my condition, as much as I would love to try TENS in the early stages of labour, it’s contraindicated, so it wouldn’t be a good idea to try. I’m also not able to have a water birth as there’s no way to be able to hoist me out of the pool in an emergency. I am, however, hoping that we get one of the rooms that has an ensuite bath in so that Alex can help me get in and out of that in the early stages of labour. Of course, this is dependant on how much monitoring little one requires. Still, we’re hoping we won’t need to be on monitoring continuously.
What if we have to go down the medical pain relief route?
As I said at the beginning, I’m allergic to most medical forms of pain relief. Outside of the hospital, the only painkiller I can take is paracetamol, so of course, that will be the first thing. I take paracetamol regularly to keep the edge off of my day to day pain levels, so, likely, I’ll just continue that regime through labour. Luckily, I’m able to tolerate fentanyl in small doses. There’s a fast-acting version that can be given if needed, but I’m hoping to avoid it. We also have the option of gas and air. I just have to be mindful of how much I take at once.
What about an epidural?
Epidural is something that has been discussed at length with various people in the team looking after us. We’ve already decided that if we need it, we’re going to try it even though it’s technically challenging because of how my spine is. Another problem is that my body doesn’t always respond to local or regional anaesthetics, which caused my thumb fusion to be done under a general last year after a regional failure where I ended up screaming in pain. However, you never know if you don’t try, and I’m willing to try anything to get the birth I want!
Did you use any alternative therapies or treatments during labour and birth? Share them in the comments for others to see!
This post contains affiliate links. This means that we receive a percentage of the revenue made from purchasing products when you click on a link. This does not affect you as the consumer or the price of the product or service. It is also not a paid for promotion or a collaboration/advert.